As the immune-evasive coronavirus variant fuels another wave of infections, here is how to get the most out of at-home testing.
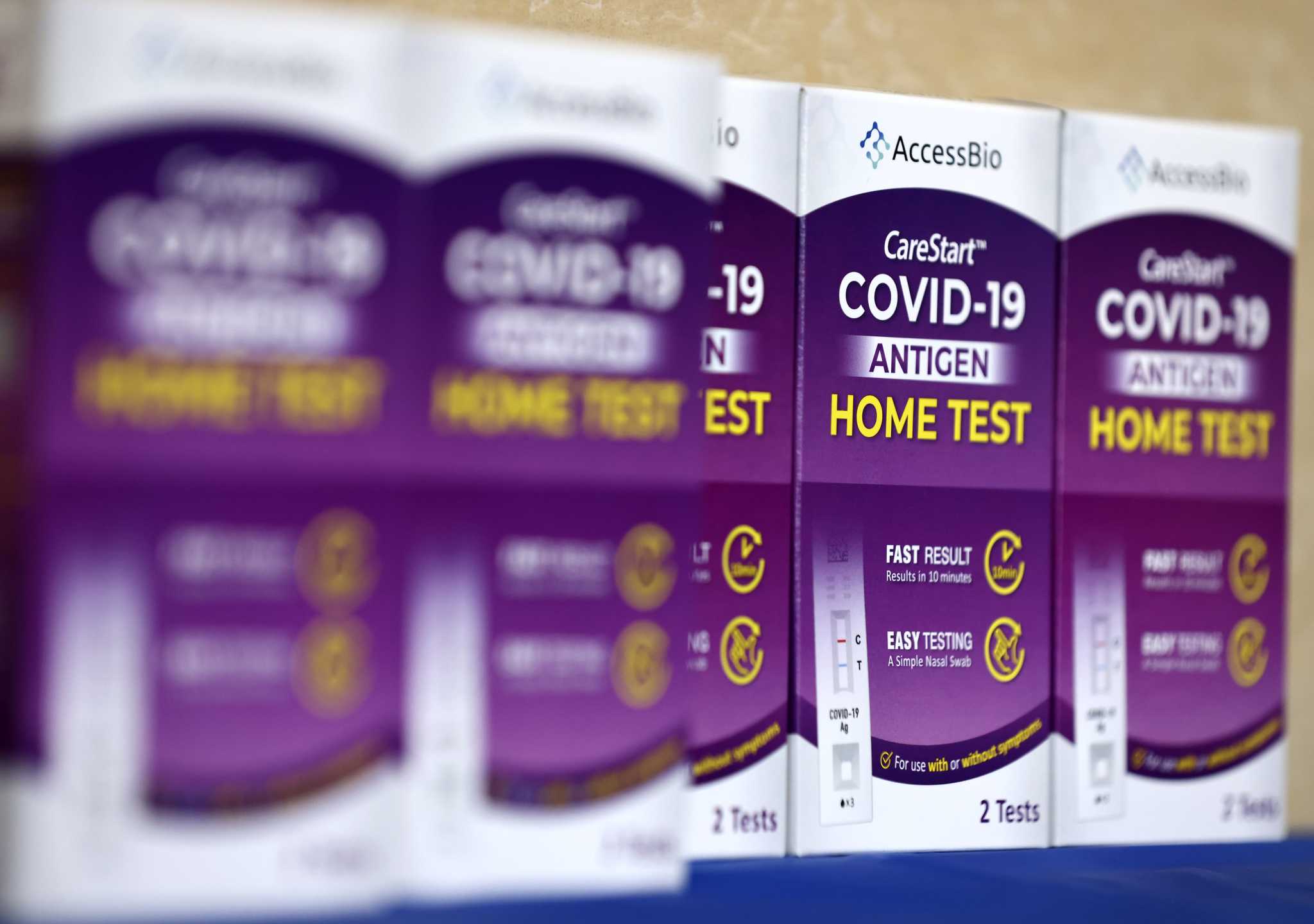
Mario Tama/Getty ImagesThe widespread availability of rapid antigen tests has made at-home COVID-19 screening quick and convenient. But federal health officials caution that these tests, while invaluable in detecting infections and curbing spread of the coronavirus, may have become less reliable due to the emergence of newer omicron variants such as JN.1.
What is the best way now to navigate testing as the Bay Area faces another winter COVID-19 surge? While familiar advice still applies, experts offer additional insights in light of the evolving nature of the virus, which can make people sick faster than it used to.
Peter Chin-Hong, an infectious disease expert at UCSF, notes that some people now test positive only three days after exposure, down from five days earlier in the pandemic.
Advertisement
Article continues below this ad
At the same time, mutations to the virus mean that test kits may not spot it for up to a week after exposure. That’s because the kits were designed for earlier variants, and while they can still sense the newer ones, a greater buildup of virus samples in the nostrils is required to trigger a positive test result.
If you test negative for COVID-19 at home, it doesn’t always mean you’re in the clear. If you swab too soon after being exposed to the virus, you may get a false negative. For newer variants, experts recommend starting to test around three days after exposure. If the result is negative, keep testing every day or two until the sixth day.
While molecular laboratory tests, such as PCR rests, are more sensitive and accurate, they typically require a visit to a clinic or doctor’s office and can be costly.
Regardless of test results, individuals feeling unwell are strongly advised to wear high-quality masks in crowded environments and to stay home to mitigate the risk of spreading germs, according to the U.S. Centers for Disease Control and Prevention. Staying up-to-date with the latest vaccines is also crucial, considering the presence of other respiratory illnesses like influenza or RSV.
“Given that hospitalizations are rising here because of holiday gatherings and decreased (waning) immunity, it is a good idea to take the usual precautions,” said Nadia Roan, a UCSF immunologist and investigator at the Gladstone Institutes. “We have a pretty big toolbox now compared to the beginning of the pandemic. They all work.”
Advertisement
Article continues below this ad
While JN.1, a descendant of the BA.2.86 omicron strain, appears more transmissible, there is no evidence it is causing more severe illness. But Roan cautions that the variant, which emerged in November, has not been fully evaluated by virologists.
The CDC reports JN.1 now constitutes approximately 62% of cases in the United States, a significant jump from 21% a month ago.
Despite a rise in Bay Area wastewater virus levels and test positivity rates — which can spot both symptomatic and asymptomatic infections — COVID-19-related hospitalizations are 22% lower than in the same period a year ago, and deaths are down 38%, federal data show.
That difference, Roan said, is likely due to an overall higher level of protection across the whole population, “whether from prior infection or vaccination, or both.” It’s also possible, she said, “that JN.1 is less virulent than the early strains of the virus.”
The most commonly reported JN.1 symptoms include congestion, cough and a sore throat. Some recent studies have also suggested a link to anxiety and insomnia, and the potential to better infect the lungs.
Advertisement
Article continues below this ad
Various factors influence the dependability of at-home antigen tests. These include the test’s sensitivity and specificity, the quality of the sample, how well the user follows the manufacturer’s instructions, the period since the person’s last exposure or symptoms, and the viral load present during testing.
Asymptomatic individuals with positive test results should self-isolate for at least five days or until obtaining a negative result.
The antiviral medication Paxlovid, effective in reducing severe illness, must be taken within five days of a positive test, emphasizing the importance of timely and accurate readings.
Despite the end of the national COVID-19 public health emergency, at-home tests remain widely available through healthcare providers, pharmacies and community organizations.
Advertisement
Article continues below this ad
Those who have been hoarding at-home test kits in anticipation of the current surge may want to check the expiration dates. The FDA approved most tests to have expiration dates ranging from approximately four to six months. Some components of the tests may degrade over time, potentially leading to inaccurate results.
Scientists have not pinpointed the precise time frame when specific kit elements lose reliability. In general, the agency recommends avoiding the use of expired tests.
Reach Aidin Vaziri: [email protected]

Dr. Debi Johnson is a medical expert and health journalist dedicated to promoting well-being. With a background in medicine, she offers evidence-based insights into health trends and wellness practices. Beyond her reporting, Dr. Debi enjoys hiking, yoga, and empowering others to lead healthier lives.