Summary: Researchers discovered a potential link between lower levels of serotonin, the “happiness” chemical, and mild cognitive impairment (MCI), which could advance our understanding of Alzheimer’s Disease (AD).
Their study indicates that individuals with MCI have significantly reduced serotonin transporter levels, a factor that might contribute to memory problems and potentially AD. This finding offers new avenues for treatment, as serotonin levels could become a target for early intervention to slow or halt disease progression.
However, the study emphasizes the correlation rather than causation and calls for further research to explore the role of serotonin in transitioning from MCI to AD.
Key Facts:
- Individuals with MCI showed up to 25% lower levels of serotonin transporters in specific brain regions compared to healthy controls.
- The study, spanning 2009-2022, included 49 volunteers with MCI and 45 healthy adults, utilizing MRI and PET scans to analyze brain changes and serotonin transporter levels.
- The researchers suggest that targeting serotonin levels might not only improve memory deficits but could also alleviate depressive symptoms, offering a potential strategy to slow AD progression.
Source: Johns Hopkins University
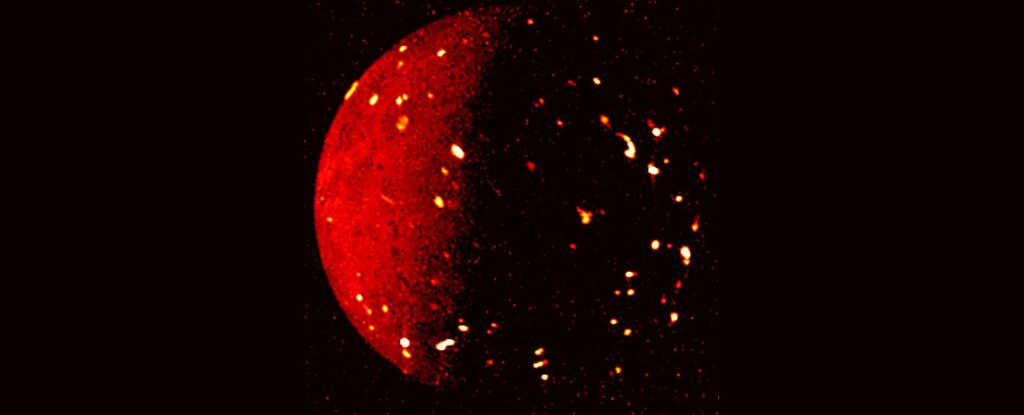
Comparing PET scans of more than 90 adults with and without mild cognitive impairment (MCI), Johns Hopkins Medicine researchers say relatively lower levels of the so-called “happiness” chemical, serotonin, in parts of the brain of those with MCI may play a role in memory problems including Alzheimer’s disease.
The findings, first published online Sept. 13 in the Journal of Alzheimer’s Disease, lend support to growing evidence that measurable changes in the brain happen in people with mild memory problems long before an Alzheimer’s diagnosis, and may offer novel targets for treatments to slow or stop disease progression.
“The study shows that people with mild cognitive impairment already display loss of the serotonin transporter. This measure that reflects serotonin degeneration is associated with problems with memory, even when we take into account in our statistical model MRI measures of neurodegeneration and PET measures of the amyloid protein that are associated with Alzheimer’s Disease,” says Gwenn Smith, Ph.D., professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine.
MCI describes the diagnostic stage between normal brain function in aging and Alzheimer’s Disease (AD). Symptoms of MCI include frequent forgetfulness of recent events, word finding difficulty, and loss of the sense of smell.
Those with MCI may stay in this stage indefinitely, or progress to more severe forms of cognitive deficits, giving urgency to the search for predictive markers, and possible early prevention interventions, investigators say.
The investigators cautioned that their study showed a correlation between lower serotonin transporter levels and memory problems in MCI, and was not designed to show causation or the role of serotonin in the progression from MCI to AD. To answer these questions, further research is needed to study over time healthy controls and individuals with MCI to demonstrate the role of serotonin in disease progression.
For the study, the Hopkins scientists recruited 49 volunteers with MCI, and 45 healthy adults ages 55 and older who underwent an MRI to measure changes in brain structure and two positron emission tomography (PET) scans of their brains at Johns Hopkins between 2009 and 2022.
The research team used PET scans to look specifically at the serotonin transporter – a neurotransmitter, or brain chemical long associated with positive mood, appetite and sleep – and to look at the amyloid-beta protein (Aβ) distribution in the brain. Aβ is thought to play a central role in the pathology of AD.
Studies in mice done at Johns Hopkins have shown that serotonin degeneration occurs before the development of widespread beta-amyloid deposits in the brain. Loss of serotonin is often associated with depression, anxiety, and psychological disorders.
Researchers found that MCI patients had lower levels of the serotonin transporter, and higher levels of Aβ than healthy controls. The MCI patients had up to 25% lower serotonin transporter levels in cortical and limbic regions than healthy controls.
In particular, they report, lower serotonin transporter levels were found in cortical, limbic, and subcortical regions of the brains in those with MCI, areas specifically responsible for executive function, emotion, and memory.
“The correlation we observed between lower serotonin transporters and memory problems in MCI is important because we may have identified a brain chemical that we can safely target that may improve cognitive deficits and, potentially, depressive symptoms,” says Smith.
“If we can show that serotonin loss over time is directly involved in the transition from MCI to AD, recently developed antidepressant medications may be an effective way to improve memory deficits and depressive symptoms and thus, may be a powerful way forward to slow disease progression.”
Researchers say future studies include longitudinal follow up of individuals with MCI to compare serotonin degeneration to the increase in and Aβ levels, as well as the increase in levels of the Tau protein that is also associated with AD compared to healthy adults. They are also studying multi-modal antidepressant drugs to treat depression and memory deficits in hopes of mitigating and halting symptoms.
Other scientists at the Johns Hopkins University School of Medicine and Johns Hopkins Bloomberg School of Public Health who contributed to this research are Jennifer Coughlin, Robert Dannals, Neda Gould, Daniel Holt, Vidya Kamath, Michael Kraut, Hiroto Kuwabara, Jeannie Leoutsakos, Martin Lodge, Ayon Nandi, Najlla Nassery, Martin Pomper, Alena Savonenko, Haijuan Yan and Mark Yoon.
All authors have no conflicts to disclose.
Funding: This research was partly supported by the National Institutes of Health.
About this Alzheimer’s disease research news
Author: Kristen Crocker
Source: Johns Hopkins University
Contact: Kristen Crocker – Johns Hopkins University
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“Serotonin Degeneration and Amyloid-β Deposition in Mild Cognitive Impairment: Relationship to Cognitive Deficits” by Gwenn Smith et al. Journal of Alzheimer’s Disease
Abstract
Serotonin Degeneration and Amyloid-β Deposition in Mild Cognitive Impairment: Relationship to Cognitive Deficits
Background: Neuropathological and neuroimaging studies have demonstrated degeneration of the serotonin system in Alzheimer’s disease (AD). Neuroimaging studies have extended these observations to the preclinical stages of AD, mild cognitive impairment (MCI). Serotonin degeneration has been observed also in transgenic amyloid mouse models, prior to widespread cortical distribution of amyloid-β (Aβ).
Objective: The present study evaluated the regional distribution of the serotonin transporter (5-HTT) and of Aβ in individuals with MCI and healthy older controls, as well as the contribution of 5-HTT and Aβ to cognitive deficits.
Methods: Forty-nine MCI participants and 45 healthy older controls underwent positron emission tomography (PET) imaging of 5-HTT and Aβ, structural magnetic resonance imaging and neuropsychological assessments.
Results: Lower cortical, striatal, and limbic 5-HTT and higher cortical Aβ was observed in MCIs relative to healthy controls. Lower 5-HTT, mainly in limbic regions, was correlated with greater deficits in auditory-verbal and visual-spatial memory and semantic, not phonemic fluency. Higher cortical A β was associated with greater deficits in auditory-verbal and visual-spatial memory and in semantic, not phonemic fluency. When modeling the association between cognition, gray matter volumes and Aβ, inclusion of 5-HTT in limbic and in select cortical regions significantly improved model fit for auditory-verbal and visual-spatial memory and semantic, but not phonemic fluency.
Conclusions: These results support the role of serotonin degeneration in the memory and semantic fluency deficits observed in MCI.

Dr. Debi Johnson is a medical expert and health journalist dedicated to promoting well-being. With a background in medicine, she offers evidence-based insights into health trends and wellness practices. Beyond her reporting, Dr. Debi enjoys hiking, yoga, and empowering others to lead healthier lives.